What Is Bigger A Skin Cell Or A Red Blood Cell
The boilerplate human adult has more than 5 liters (half dozen quarts) of blood in his or her body. Claret carries oxygen and nutrients to living cells and takes away their waste products. It likewise delivers allowed cells to fight infections and contains platelets that can form a plug in a damaged blood vessel to prevent blood loss.
Through the circulatory system, blood adapts to the torso's needs. When you are exercising, your heart pumps harder and faster to provide more blood and hence oxygen to your muscles. During an infection, the blood delivers more than immune cells to the site of infection, where they accrue to ward off harmful invaders.
All of these functions make blood a precious fluid. Each twelvemonth in the USA, thirty million units of blood components are transfused to patients who demand them. Claret is deemed so precious that is also called "red gold" because the cells and proteins it contains can be sold for more than the price of the same weight in gold.
This chapter introduces the components of blood.
Blood contains cells, proteins, and sugars
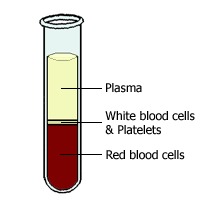
If a examination tube of blood is left to stand for one-half an hour, the blood separates into three layers equally the denser components sink to the bottom of the tube and fluid remains at the tiptop.
The straw-colored fluid that forms the top layer is chosen plasma and forms about 60% of blood. The middle white layer is equanimous of white blood cells (WBCs) and platelets, and the bottom red layer is the red blood cells (RBCs). These bottom two layers of cells form virtually forty% of the claret.
Plasma is mainly water, but it also contains many important substances such equally proteins (albumin, clotting factors, antibodies, enzymes, and hormones), sugars (glucose), and fat particles.
All of the cells found in the blood come from os marrow. They begin their life every bit stem cells, and they mature into three chief types of cells— RBCs, WBCs, and platelets. In plow, there are three types of WBC—lymphocytes, monocytes, and granulocytes—and three chief types of granulocytes (neutrophils, eosinophils, and basophils). Come across them in activeness in "Meet the blood cells".
![]()
See a effigy of all the cellular elements of blood in Janeway & Traver'due south Immunobiology
A sample of claret tin be further separated into its individual components by spinning the sample in a centrifuge. The force of the spinning causes denser elements to sink, and further processing enables the isolation of a particular protein or the isolation of a particular type of blood prison cell. With the utilise of this method, antibodies and clotting factors can be harvested from the plasma to treat immune deficiencies and bleeding disorders, respectively. Likewise, RBCs can be harvested for blood transfusion.
Red claret cells send oxygen
![]()
Every second, two-three million RBCs are produced in the bone marrow and released into the circulation. Also known as erythrocytes, RBCs are the about common blazon of cell institute in the blood, with each cubic millimeter of claret containing four-6 1000000 cells. With a diameter of only 6 µm, RBCs are small enough to clasp through the smallest blood vessels. They circulate around the body for up to 120 days, at which point the quondam or damaged RBCs are removed from the circulation by specialized cells (macrophages) in the spleen and liver.
In humans, every bit in all mammals, the mature RBC lacks a nucleus. This allows the cell more than room to shop hemoglobin, the oxygen-bounden poly peptide, enabling the RBC to transport more oxygen. RBCs are besides biconcave in shape; this shape increases their surface surface area for the improvidence of oxygen across their surfaces. In non-mammalian vertebrates such equally birds and fish, mature RBCs exercise have a nucleus.
If a patient has a depression level of hemoglobin, a condition chosen anemia, they may appear pale because hemoglobin gives RBCs, and hence blood, their red color. They may too tire easily and feel short of breath because of the essential role of hemoglobin in transporting oxygen from the lungs to wherever it is needed around the body.
White blood cells are part of the immune response
WBCs come in many unlike shapes and sizes. Some cells take nuclei with multiple lobes, whereas others contain one large, round nucleus. Some contain packets of granules in their cytoplasm then are known equally granulocytes.
Despite their differences in appearance, all of the various types of WBCs have a part in the immune response. They circulate in the claret until they receive a point that a function of the body is damaged. Signals include interleukin 1 (IL-1), a molecule secreted by macrophages that contributes to the fever of infections, and histamine, which is released by circulating basophils and tissue mast cells, and contributes to allergic reactions. In response to these signals, the WBCs get out the blood vessel by squeezing through holes in the blood vessel wall. They migrate to the source of the betoken and assist begin the healing process.
Individuals who accept low levels of WBCs may have more and worse infections. Depending upon which WBCs are missing, the patient is at risk for different types of infection. For example, macrophages are specially good at swallowing bacteria, and a deficiency in macrophages leads to recurrent bacterial infections. In contrast, T cells are particularly skilled in fighting viral infections, and a loss of their part results in an increased susceptibility to viral infections.
Neutrophils digest leaner
![]()
Neutrophils are also known as polymorphonuclear cells because they contain a nucleus whose shape (morph) is irregular and contains many (poly) lobes. They also vest to a group of WBCs known as granulocytes because their cytoplasm is dotted with granules that contain enzymes that helps them digest pathogens.
Monocytes become macrophages
![]()
Monocytes are young WBCs that circulate in the blood. They develop into macrophages after they accept left the blood and migrated into tissue. At that place they provide an firsthand defense because they can engulf (phagocytose) and digest pathogens before other types of WBCs achieve the area.
In the liver, tissue macrophages are called Kupffer cells, and they specialize in removing harmful agents from claret that has left the gut. Alveolar macrophages are in the lungs and remove harmful agents that may have been inhaled. Macrophages in the spleen remove quondam or damaged red blood cells and platelets from the circulation.
Macrophages are also "antigen-presenting cells", presenting the strange proteins (antigens) to other allowed cells, triggering an immune response.
Lymphocytes consist of B cells and T cells
![]()
Lymphocytes are round cells that incorporate a unmarried, large round nucleus. There are two main classes of cells, the B cells that mature in the bone marrow, and the T cells that mature in the thymus gland.
Once activated, the B cells and T cells trigger different types of allowed response. The activated B cells, besides known equally plasma cells, produce highly specific antibodies that demark to the agent that triggered the immune response. T cells, called helper T cells, secrete chemicals that recruit other allowed cells and aid coordinate their attack. Another group, chosen cytotoxic T cells, attacks virally infected cells.
Platelets help blood to clot
![]()
Platelets are irregularly shaped fragments of cells that circulate in the claret until they are either activated to grade a blood clot or are removed by the spleen. Thrombocytopenia is a condition of depression levels of platelets and carries an increased take chances of bleeding. Conversely, a high level of platelets (thrombocythemia) carries an increased risk of forming inappropriate blood clots. These could deprive essential organs such as the eye and brain, of their blood supply, causing heart attacks and strokes, respectively.
Equally with all the cells in the blood, platelets originate from stem cells in the bone marrow. The stem cells develop into platelet precursors (called megakaryocytes) that "shed" platelets into the bloodstream. There, platelets circulate for about 9 days. If they encounter damaged blood vessel walls during this fourth dimension, they stick to the damaged area and are activated to class a blood clot. This plugs the hole. Otherwise, at the terminate of their life bridge they are removed from the apportionment by the spleen. In a diverse number of diseases where the spleen is overactive, e.g. rheumatoid arthritis and leukemia, the spleen removes too many platelets, leading to increased haemorrhage.
Your consummate blood count
A complete blood count (CBC) is a simple blood exam that is commonly ordered as function of a routine medical assessment. As the name suggests, it is a count of the unlike types of cells found in the claret. The test can diagnose and monitor many different diseases, such equally anemia, infection, inflammatory diseases, and malignancy. Tabular array i gives an example of CBC values, merely note that the reference ranges and the units used may differ, depending upon the laboratory that carried out the test.
Red blood prison cell count detects anemia
A CBC measures the post-obit features of RBCs:
-
the total amount of hemoglobin (Hb) in the blood
-
the number of RBCs (RBCs)
-
the average size of a RBC (MCV)
-
the corporeality of space RBCs take up in the blood (hematocrit)
The CBC also includes information about RBCs that is calculated from the other measurements, e.g., the amount (MCH) and concentration (MCHC) of hemoglobin in RBCs.
The number of RBCs and the amount of hemoglobin in the claret are lower in women than in men. This is because of the menstrual loss of blood each month. Below a certain level of hemoglobin, a patient is said to be anemic, suggesting a clinically meaning drop in oxygen carrying chapters. Anemia is not a diagnosis but a symptom of an underlying disease that has to be investigated.
A clue to the cause of anemia is the average size of RBC (mean corpuscular volume, MCV). Causes of a high MCV include a deficiency of B12 or folate vitamins in the diet. B12 is institute in red meat therefore, a deficiency of B12 is specially common in vegetarians and vegans. Conversely, folate is plentiful in fresh leafy light-green vegetables, therefore, a deficiency of folate is common in the elderly, who may have a poor diet.
Low MCV anemia is mutual and may be a issue of hereditary blood disorders, such as thalassemia, simply is most often acquired past a deficiency of atomic number 26. For example, women of reproductive age may lose too much iron through heavy menstrual bleeding and are prone to this form of anemia, known as iron-deficiency anemia.
Hematocrit is the percentage of RBCs in relation to the total book of blood
The hematocrit measures the fraction of the claret that is made upwards of RBCs. It reflects the combination of the total number of RBCs, and the book that they occupy.
One of the changes seen in pregnancy is a drop in hematocrit. This occurs because although the production of RBCs does not modify greatly, the plasma volume increases, i.e., the RBCs are "diluted". Alternatively, a low hematocrit can reflect a drop in RBC production by the bone marrow. This may be attributable to bone marrow affliction (damage by toxins or cancer) or due to a subtract in erythropoietin, a hormone secreted by the kidney that stimulates RBC production. Decreased RBCs may also exist the issue of a reduced life span of the RBCs (due east.1000., chronic haemorrhage).
A high hematocrit value may truly reflect an increase in the fraction of RBCs (e.g., increased erythropoietin attributable to a tumor of RBCs called polycythemia rubra vera), or it may reflect a drop in the plasma component of the blood (e.g., fluid loss in burn victims).
The number of WBCs increases in infection and tumors
The WBC count is a count of the number of WBCs establish in one cubic millimeter of claret.
An increased number of WBCs is most commonly caused by infections, such as a urinary tract infection or pneumonia. It may too be acquired by WBC tumors, such as leukemia.
A decreased number of WBCs is caused by the bone marrow failing to produce WBCs or by an increased removal of WBCs from the circulation by a diseased liver or an overactive spleen. Bone marrow failure may be caused by toxins or by the normal bone marrow cells being replaced by tumor cells.
The WBC differential office of the CBC breaks downwardly the WBCs into 5 different types: neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Finding out the count of each type of WBC gives more than information near the underlying problem. For example, in the early stages of an infection, about of the increase in WBCs is attributable to the increase in neutrophils. As the infection continues, lymphocytes increase. Worm infections can trigger an increase in eosinophils, whereas allergic conditions, such equally hay fever, trigger an increase in basophils.
The number of platelets indicates whether bleeding or clotting is likely
Normally, one cubic millimeter of blood contains between 150,000 and 400,000 platelets. If the number drops beneath this range, uncontrolled bleeding becomes a risk, whereas a rise above the upper limit of this range indicates a risk of uncontrolled blood clotting.
Hemoglobin binds oxygen
Hemoglobin is the oxygen-carrying poly peptide that is found within all RBCs. It picks up oxygen where information technology is abundant (the lungs) and drops off oxygen where it is needed around the body. Hemoglobin is as well the pigment that gives RBCs their red color.
Heme groups and globins
Every bit its name suggests, hemoglobin is composed of "heme" groups (iron-containing rings) and "globins" (proteins). In fact, hemoglobin is equanimous of four globin proteins—two alpha chains and two beta chains—each with a heme grouping. The heme group contains 1 atomic number 26 atom, and this can bind one molecule of oxygen. Because each molecule of hemoglobin contains 4 globins, it can bear up to 4 molecules of oxygen.
Hemoglobin transports oxygen
In the lungs, a hemoglobin molecule is surrounded by a high concentration of oxygen, therefore, information technology binds oxygen. In active tissues, the oxygen concentration is lower, so hemoglobin releases its oxygen.
This behavior is much more effective because the hemoglobin––oxygen bounden is "co-operative". This means that the bounden of i molecule of oxygen makes it easier for the binding of subsequent oxygen molecules. Also, the unbinding of oxygen makes it easier for other oxygen molecules to be released. This means that the response of hemoglobin to the oxygen needs of agile tissues is much quicker.
Aside from the oxygen saturation of hemoglobin, other factors that influence how readily hemoglobin binds oxygen include plasma pH, plasma bicarbonate levels, and the pressure of oxygen in the air (high altitudes in detail).
The molecule two,3-disphosphoglycerate (2,3-DPG ) binds to hemoglobin and lowers its affinity for oxygen, thus promoting oxygen release. In individuals who have become acclimatized to living at loftier altitudes, the level of 2,3-DPG in the blood increases, allowing the delivery of more oxygen to tissues under depression oxygen tension.
Fetal hemoglobin
Fetal hemoglobin differs from developed hemoglobin in that it contains two gamma chains instead of two beta chains. Fetal hemoglobin binds oxygen with a much greater affinity than adult hemoglobin; this is an reward in the womb considering it allows fetal claret to extract oxygen from maternal blood, despite its low concentration of oxygen.
Normally, all fetal hemoglobin is replaced by adult hemoglobin past the time of nativity.
Breaking downwards hemoglobin
Former or damaged RBCs are removed from the apportionment past macrophages in the spleen and liver, and the hemoglobin they incorporate is cleaved down into heme and globin. The globin poly peptide may be recycled, or broken down further to its constituent amino acids, which may be recycled or metabolized. The heme contains precious fe that is conserved and reused in the synthesis of new hemoglobin molecules.
During its metabolism, heme is converted to bilirubin, a yellow pigment that can discolor the skin and sclera of the centre if it accumulates in the blood, a condition known as jaundice. Instead, the plasma poly peptide albumin binds to bilirubin and carries it to the liver, where it is secreted in bile and as well contributes to the color of feces.
Jaundice is one of the complications of an incompatible blood transfusion. This occurs when the recipient's immune arrangement attacks the donor RBCs equally being foreign. The rate of RBC destruction and subsequent bilirubin product tin exceed the capacity of the liver to metabolize the bilirubin produced.
Hemoglobinopathies
Hemoglobinopathies form a group of inherited diseases that are caused by mutations in the globin bondage of hemoglobin. Sickle prison cell anemia is the most common of these and is attributable to a mutation that changes one of the amino acids in the hemoglobin beta chain, producing hemoglobin that is "fragile". When the oxygen concentration is low, RBCs tend to become distorted and "sickle" shaped. These deformed cells can block small blood vessels and harm the organs they are supplying. This can be very painful, and if not treated, a sickle cell crisis can be fatal.
Another inherited anemia that particularly affects individuals of Mediterranean descent is thalassemia. A mistake in the production of either blastoff or beta globin chains causes a range of symptoms, depending on how many copies of the blastoff and beta genes are affected. Some individuals may be carriers of the disease and have no symptoms, whereas if all copies of the genes are lost, the disease is fatal.
The porphyrias are a group of inherited disorders in which the synthesis of heme is disrupted. Depending upon the stage at which the disruption occurs, in that location are a range of neurological and gastrointestinal side effects. King George III of England ("the madness of Male monarch George") was one of the most famous individuals who suffered from porphyria.
Source: https://www.ncbi.nlm.nih.gov/books/NBK2263/
Posted by: lononmarted1980.blogspot.com


0 Response to "What Is Bigger A Skin Cell Or A Red Blood Cell"
Post a Comment